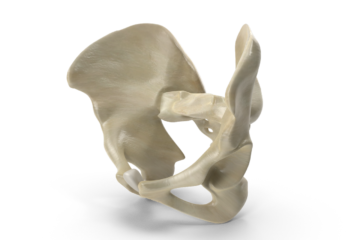
‘Arthritis’ usually refers to osteoarthritis, the most commonly diagnosed type of arthritis, and the most common joint disorder in Canada and the US. Unless you are referred to a rheumatologist, odds are you are dealing with osteoarthritis. Osteoarthritis (OA) can affect any joint, but most often occurs in the knees, hips, lower back and neck, fingers, and the bases of the thumb and big toe. Normally joints have a layer of smooth cartilage covering the end of each bone. This allows the joint to glide smoothly and provides a cushion between the bones. In OA, the cartilage breaks down, which causes pain, swelling, and difficulty moving the joint. Over time, the bones themselves may start to break down and develop growths called spurs. In the final stages of OA, the cartilage wears away and bone rubs against bone, which leads to joint damage and more pain. This is the point where a joint replacement is usually recommended.

What causes osteoarthritis?
Many different factors contribute to the development of osteoarthritis. Age is by far the biggest contributing factor, with the prevalence of OA increasing in each age group. In Canada, approximately 13% of adults aged 20 and over live with diagnosed OA, however that percentage increases each decade to >45% in adults over 80 years of age. The main contributing factors to the development of OA are as follows
- Age
- Female gender
- Obesity (particularly in knee and hip OA)
- Anatomical factors
- Muscle weakness
- Joint injury

How can osteoarthritis be managed?
The first step is prevention. To reduce the risk of developing osteoarthritis, or to delay its onset, it is important to maintain a healthy active lifestyle. This means maintaining a healthy body weight, keeping joints healthy and muscles strong through physical activity, and protecting joints from injury and overuse.
While there is no cure for osteoarthritis, symptoms can be managed to relieve pain, prevent or reduce further joint damage, improve mobility, and delay the need for surgery.
Pain medication, including antiinflammatories can be helpful. Non-pharmaceutical pain control methods can also be beneficial – these include (but are not limited to) acupuncture, thermotherapy (heat and cold therapy), cupping, neuromuscular electrical stimulation (such as TENS or IFC), ultrasound therapy, massage therapy, and manual therapy (including physiotherapy mobilizations).
Exercise is also a key component of osteoarthritis management. In addition to weight management to prevent increased strain on the joints of the lower body, exercise itself can help slow down or even halt the progression of OA. Therapeutic exercise can improve range of motion, reduce pain, improve joint biomechanics, and help strengthen surrounding muscles to offload the affected joint.
Sometimes OA is so advanced that joint replacement is the only option. This is most commonly performed for the knee and the hip joint. It is important to maximize your range of motion and strength before and after surgery to ensure the best outcome.
Wondering what you can do to help manage your osteoarthritis? Speak to a physiotherapist! Physiotherapists are specialists in pain management, exercise prescription, and all things osteoarthritis!