At KinaHEALTH, the difference lies in the way we approach each and every treatment. We strongly believe that hands-on physiotherapy treatment by a skilled physiotherapist is central to your successful and effective recovery. This means no machines, no double-booking, and most importantly no open treatment spaces. Each physiotherapy appointment takes place in one of our private treatment rooms with just you and your physiotherapist. This approach to treatment ensures that you have your therapists undivided attention and the focus is entirely on you two working together to achieve your goals.
We believe that building trust with your physiotherapist is very important to an effective recovery. That's why every one of your appointments at KinaHEALTH, from your assessment to each follow-up treatment, will be entirely one-on-one with your physiotherapist.

You treatments will be comprised of various hands-on techniques as the primary means of treatment at KinaHEALTH. You will not be left alone connected to a machine or to perform exercises by yourself.
When addressing your health and well-being concerns, privacy is important. At KinaHEALTH you will always be cared for in one of our private treatment rooms. That means no wide open areas separated by curtains, no overhearing other conversations, and nobody watching you receive your treatments.

When identifying the root cause of an injury, it is important to consider the myofascial, articular (joint), neural, visceral (organ), as well as cognitive and emotional components. This ensures we address all influencing factors to efficiently relieve symptoms and restore optimal movement.
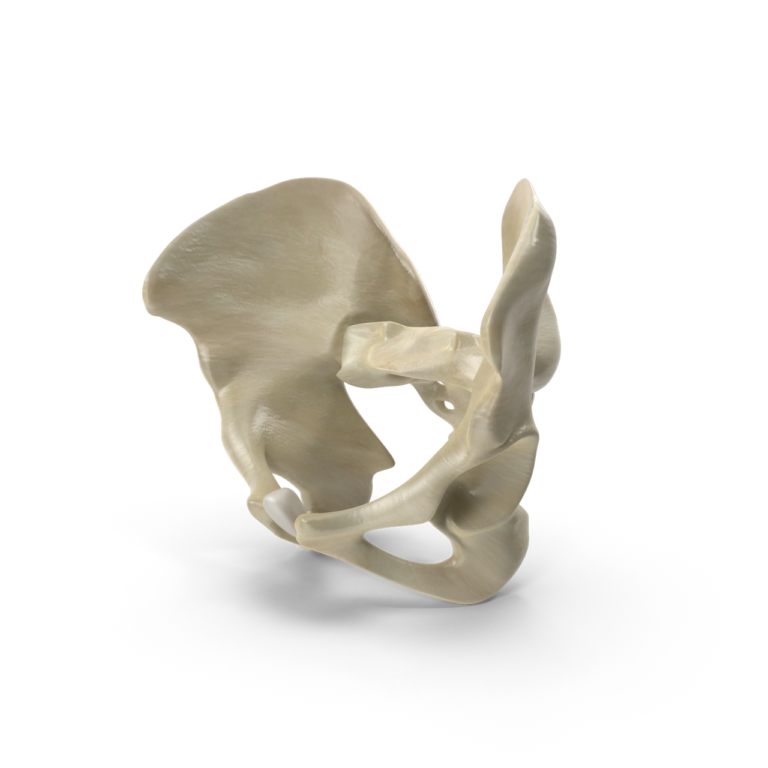
It is also equally important to take into account the connection of the deeper structures of the pelvis and core system to the whole body. At KinaHEALTH we provide you with the benefit of pelvic health knowledge and its often missed contribution to orthopaedic complaints.
This is not a full or exhaustive list of conditions treated. If you have any questions about an injury that is not on the list, please contact the clinic to discuss your condition and whether or not physiotherapy may be beneficial to you. You may also schedule a 15 minute complimentary phone call with a therapist.
The pelvis as well as the abdomen and its contents is the centre of your body; it’s where we balance, sit, derive pleasure, and grow our babies.
The pelvic floor can be imagined as a bowl of muscles in the bottom of your pelvis. We all sit and move on these muscles every single day. Dysfunctions within can impact everything from strength, mobility and performance to digestion, elimination and reproduction.
So, what does your pelvic floor do? It provides:
CONTINENCE. They are the reason we do not leak urine, gas or stool.
SUPPORT. They hold up our pelvic organs including our bladder, uterus and rectum.
CORE. Move over abs. These key muscles are the foundation of your core, which supports your overall strength, balance and function.
ENJOYABLE SEX. They are the reason we can participate in pleasure, become aroused and achieve orgasm.
CIRCULATION. These muscles create a pumping action that assists blood and lymphatic drainage helping to keep our tissue fluids in balance.
Our highly trained pelvic health Physiotherapist has years of experience working with conditions that affect bladder, bowel, reproductive, sexual, and abdominal-pelvic health in women and men.

Preparing for labour and delivery, incontinence, constipation, pubic bone/sacroiliac/tailbone pain, low back pain, sciatica, rib pain, abdominal separation (diastasis recti), weakened core and/or pelvic floor, cesarean and episiotomy scars, swelling/water retention, varicose veins, tendonitis, carpal tunnel, and more;
Support and education on continued participation in physical activity during pregnancy as well as safe return to activities and sport postpartum.

WHAT IS IT?
It is a treatment technique involving the use of a thin, solid filament needle to deactivate and/or desensitize trigger points in muscles without injecting any substance (hence “dry”). Myofascial trigger points (commonly referred to as muscle knots) are taut bands of muscle within a larger muscle and can contribute to pain, decreased mobility or flexibility, and decreased muscle function. Dry needling these trigger points can help “reset” a muscle by decreasing pain and dysfunction. When used in combination with therapeutic exercise, dry needling can be used to help retrain and re-establish more appropriate movement patterns
To put it simply, dry needling is a very unique sensation. Due to the extremely thin size of the needle itself, it is often not felt at all. Most of the sensation resulting from dry needling originates from the muscle itself reacting to the technique. As the needle encounters trigger points within the muscle, a “twitch” response may be elicited. This response may feel like a quick, sudden burst of electricity in the muscle.
Though the process of dry needling can be uncomfortable, you will always be in control. If you choose to stop or require a break, simply ask your physiotherapist.
Luckily, dry needling is a quick and effective process, taking only approximately 10-15 seconds to complete a location.
Your therapist is properly trained and rostered (certified) to perform the dry needling technique. As such, your therapist has trained to perform dry needling safely and with sterile technique. New sterile and disposable one time use needles are used every time. The most common side effect from dry needling is mild soreness following the procedure, lasting up to 24 hours. On occasion, a small, dime to nickel-sized bruise can also appear following dry needling.
Your therapist is also well-educated in the possible precautions, contraindications and complications that may arise, and these will be discussed with you prior to the procedure. Some conditions and cases may not be appropriate for Dry Needling, so it is just as important that we recognize and discuss what CAN’T be treated by Dry Needling as well as what CAN.
Physical therapists who perform Functional Dry Needling consider every muscle and its relationship to the body, seeking to address these tissues for improved function and pain.
The practice of acupuncture by acupuncturists and the performance of dry needling by physical therapists differ in terms of historical, philosophical, indicative, and practical context. The performance of modern dry needling by physiotherapists is based on western neuroanatomy and modern scientific study of the musculoskeletal and nervous system. Physiotherapists who perform dry needling do not use traditional acupuncture theories or acupuncture terminology.
Acupuncture is a technique used to encourage natural healing, reduce or relieve pain, reduce stress, and improve function. Acupuncture can be applied to almost any part of the body, depending the goal and its intended purpose.
Acupuncture treatments are administered by specially trained therapists at our clinic. Thin, sterile needles are gently placed in precise locations depending on the area of concern in order to promote natural blood-flow. These needles also stimulate the brain and spinal cord to produce natural pain-relieving chemicals to assist the body’s natural healing process and offer pain relief.


Cupping Therapy has been used for centuries by people all over world as a safe, comfortable and incredibly effective treatment for many health issues. Contemporary cupping methods, like dynamic cupping, are used to decompress and optimize balance and mobility within the body.
Dynamic cupping increases circulation reduces inflammation and reduces muscle tension by using a combination of massage movements, joint movements and negative pressure.
Manual therapy is a term used to describe a specialized form of hands-on treatment used by physiotherapists to treat muscular and skeletal aches and pain. Manual therapy focuses on reducing and eliminating pain by restoring the body’s natural movements using external forces and guides. Manual therapy primarily involves various forms of mobilizations and manipulations of soft tissues (such as ligaments, tendons, and muscles) as well as joints, such as the spine, shoulder, knee, hip, ankle, etc.
Manual therapy can be used to reduce pain and restore function, as well as improve range of motion following surgery, immobilizations, casting, or an injury. It can be beneficial for both acute pain (recent injuries, trauma, sports related accidents) as well as chronic pain that has been a concern for quite some time.


A concussion, also referred to as a mild traumatic brain injury, occurs following a direct or indirect impact to the head. Concussions can also result from a shaking or rapid movement of the head or body.
For many individuals, symptoms occur within the first 7 to 10 days and resolve completely within 2 to 4 weeks of the date of the initial injury.
Post-concussion syndrome is a complex disorder in which one or many symptoms of a concussion — such as headaches or dizziness among others — persist for weeks, months, and sometimes years following the initial injury that caused the concussion.
Post-concussion symptoms can include headaches, dizziness, fatigue, irritability, anxiety, insomnia, loss of concentration and/or memory, ringing in the ears, blurry vision, and noise and/or light sensitivity.
Post-concussion physiotherapy seeks to identify the underlying problems and triggers that linger following the initial concussion. Your physiotherapist will design personalized treatments and a home exercise program to slowly stimulate your brain to adapt and heal in order to decrease and eventually eliminate any remaining signs and symptoms.
Anyone suffering from signs or symptoms of a concussion more than 10-14 days following the initial injury.
The vestibular system is a sensory system which is responsible for providing our brain with information about head position, motion, and spatial orientation. It is essential for maintaining balance, equilibrium, and gaze stability as we move through our environment. A dysfunction in this system can cause nystagmus (involuntary movements of the eyes), vertigo, dizziness, nausea, imbalance or ataxia, and compromised gaze stability.
The peripheral vestibular system – which refers to the structures in your inner ear that detect movement and relationship to gravity – communicates directly with the central vestibular processing centers within the brain. The brain also takes in information from our eyes, muscles, and joints and sends out messages to control eye and body position. This complex network of signals is the reason our vision doesn’t go blurry when we turn our head and we don’t fall over when we close our eyes.

Vestibular rehabilitation is all about dizziness, vertigo, and balance.
DIZZINESS is an overarching term used to describe a variety of sensations (light headed, swaying, feeling disorientated etc.).
VERTIGO is a specific type of dizziness defined as the illusion of movement occurring in the environment (where the world seems to move around you, even though you know it to be still.)
Vertigo and dizziness are not interchangeable terms – and because the causes of dizziness are so varied, it is important to have a medical assessment prior to initiating treatment – to ensure you are getting the correct treatment based the cause of your dizziness.
– Benign Paroxysmal Positional Vertigo (BPPV)
– Head trauma: whiplash, concussion
– Vestibular system degeneration (age related)
– Vestibular neuritis/labyrinthitis
– Endolymphatic hydrops (e.g. Meniere’s Disease)
– Ototoxicity, barotrauma, acoustic neuroma
BENIGN PAROXYSMAL POSITIONAL VERTIGO (BPPV) – is the most common cause of vertigo arising from a peripheral vestibular disorder. It is most common in people over the age of 60, however can be predisposed due to head trauma in a younger population.
The cause is currently unknown, but BPPV occurs when the otoconia (small crystals in your inner ear) are displaced from their usual location in the utricle and float into one or more of the semicircular canals. Symptoms are provoked by looking up, lying down flat quickly, bending forward, and rolling in bed, and usually settle within a few seconds to a few minutes. Assessment and diagnosis is simple, and treatment can take a few as 1-3 sessions.
OTHER VESTIBULAR CAUSES OF DIZZINESS AND VERTIGO – such as neuritis/labyrinthitis, head or ear trauma, acoustic neuroma, and Meniere’s Disease can cause ongoing issues with gaze stability, motion sensitivity, compromised balance and postural control, and physical deconditioning. Each of these areas can be addressed with an individualized treatment plan. The treatment program is symptom-driven, and a home exercise program is essential to success. The most important thing to know is that while you can make yourself feel worse (by doing movements and activities that provoke your symptoms), you can’t make the problem any worse. In vestibular rehab, what makes you a little bit dizzy is good for you! This is how your brain and body adapt and learn to compensate for dysfunction within the vestibular system. The brain is most plastic (meaning flexible and ready to learn) shortly after an injury to the vestibular system (peripheral or central). The earlier you can get treatment from a trained professional, the better the prognosis!

WHAT IS IT?
The Acronym TMJ refers to the temporo-mandibular joint or what we commonly refer to as our jaw. If you suffer from TMJ pain, you know that it can be debilitating. In a majority of cases, physiotherapy should be considered the first line of defence for the treatment of TMJ dysfunctions.
A great Physiotherapist will do a thorough assessment of your particular TMJ problem and match the treatment plan to the cause of your symptoms.
The TMJ is a complex joint between the jaw bone and the skull bone. In order to function correctly both sides of the joint must be able to fully open. This movement is broken down into two phases. We have a rotational phase where the articulating surfaces of the jaw bone spins inside the joint and a translational phase where the jaw bone and a disc glide forward. If all of this movement is not coordinated well it can cause misalignment of the jaw and painful symptoms.
Your TMJ can become injured in a variety of ways that result in painful movement, or misalignment of the jaw.
TRAUMA – Some people sustain a trauma to the joint which results in an absence of stability or after a scarring process resulting in stiffness of one of the TMJ joints. The uneven movement can then lead to accelerated wear and tear of the joint structures.
GRINDING – Your dentist may have mentioned that you are grind your teeth at night and recommended a night guard to protect your teeth from wear. That repeated grinding and clenching of the jaw can have a negative effect on your TMJ joints. This can lead to joint or disc injury as well as muscle spasm.
POSTURE – Forward head posture will place the tops of the jaw bone deeper into their sockets, which may be a source of pain. That oh-so-common slouched sitting that all of us are guilty of at some point in our day; it’s not just bad for the lower back, but also the neck and jaw! This posture creates altered length-tension relationships of the muscles attached to the jaw. The correction of your posture and of this muscle imbalance to restore proper length tension relationships has a great effect on reducing pain, clicking, and deviation of jaw movement.
Most people who seek help for their TMJ dysfunctions have a hard time identifying one specific incident. They will typically describe a condition that came on slowly and gets worse over time. With the help of a physiotherapist, you will be able to identify the likely causes and address them accordingly.
TMJ symptoms can vary between mild or quite severe. At times, they can progress to the point where patients have a difficult time eating solid food. Below is a list of common symptoms that patients experience when dealing with TMJ dysfunction.
IMPROVING TMJ JOINT MOBILITY – If a patient is assessed to have TMJ arising from an immobile TMJ joint (usually as a result of some past physical trauma that resulted in stiffness) the physiotherapist can use manual therapy techniques to get the immobile TMJ moving properly again. They will then prescribe specific stretches that will help you to maintain the range of motion improvement between visits.
REDUCING TMJ MUSCLE SPASM – Physiotherapists are anatomy experts and understand how to assess the muscles of your TMJ. Often we find that muscle spasm preventing the TMJ joint from recovering. Manual therapy techniques to reduce spasm will help to improve joint alignment and movement, ultimately resulting in less pain!
STRENGTHENING FOR HYPERMOBILE TMJ JOINTS – Some patients have a TMJ joint that moves WAY too easily, way too much or in a poor pattern. Your physiotherapist can recognize this problem and help with treatments and exercises that strengthen weak muscles and improve your natural movement patterns.
POSTURAL TRAINING – Changing that forward head posture makes a big difference for some people who suffer from TMJ dysfunction. We teach patients how to strengthen postural muscles and lengthen shortened tissues so that they can improve their head position. Your Physiotherapist will also make suggestions that will help set up your workstation, car or anywhere else you spend a lot of time sitting to promote a better body position.
PAIN RELIEF FOR TMJ DYSFUNCTION – When patients are in a lot of pain and just need some relief so that they can begin to make the changes outlined above, a physiotherapist can relieve the pain with thermal modalities, acupuncture and gentle manual therapy.
Physiotherapists trained in pediatric physiotherapy are experienced in treating babies, toddlers, and children for a variety of conditions. Whether it’s helping your child reach their next motor milestone due to developmental delay, treating your baby’s torticollis, or simply helping your young athlete recover from an sports injury, physiotherapy tailored to babies and children is the best way to ensure their safe and effective recovery.

The two most common reason women will consult for breast health is in the instance of a blocked milk duct or during their breast cancer journey.
BLOCKED MILK DUCT
Breastfeeding issues can arise from problems affecting either the baby or the mother. One common problem for new moms is the development of blocked milk ducts. Blocked milk ducts can be painful and distressing. By following good practices, you can both reduce your risk of blocked ducts, and also quickly alleviate any blockage. In difficult cases blocked milk ducts can be treated effectively with therapeutic ultrasound and manual massage techniques provided by an experienced Registered Physiotherapist.
The lactating breast produces milk and transports it via an intricate network of ducts. Unfortunately, for some lactating women the duct can become blocked and the various causes for these blockages can be determined with your physiotherapist

For more ideas please visit www.CanadianBreastFeedingFoundation.org
If the plugged duct remains blocked for more than 2-3 days, seek professional help. A physiotherapists with experience treating blocked milk ducts can help by:

CLARIFYING BREAST CANCER REHABILITATION
Being diagnosed with breast cancer is often life changing. All of your energy and focus will initially be channeled at medical treatments and surgeries for breast cancer but may be unaware of the physical impairments that can result.
Clients can experience further stress and anxiety when faced with their declining level of function, independence and quality of life and at the same time experience higher levels of pain and/or disability. We are here to offer you the resources or tools to help you return to a state of normalcy.
We address causes of dysfunction post breast cancer surgery by completing:
Access to healthcare services can make all the difference in the world, which is why we continue to strive to improve access to care and provide people the care they need at this time. If in-person services aren’t advisable due to health or because of access reasons you can connect remotely a member of our team for virtual care, which uses video conference and/or the telephone to provide services at a distance. Our virtual service is easy to use, private, and, most of all, convenient.